Doorenbos to lead NIH study on sickle cell pain management
body

Researchers at the UIC College of Nursing will lead a $7.1 million, five-year national study to determine the effectiveness of acupuncture and guided relaxation for people with chronic pain from sickle cell disease.
Nursing collegiate professor Ardith Doorenbos will lead a team of researchers on the National Institutes of Health grant, which is part of its Helping to End Addiction Long-term Initiative, or NIH HEAL. The initiative aims to improve prevention and treatment strategies for opioid misuse and addiction and to enhance pain management.
“The opioid crisis in the U.S. is very severe, and some states have had more deaths from opioid overdoses than from car accidents. We’re trying to do what we can to reduce opioid use in the sickle cell disease population who have high pain levels and opioid use. If we can find ways to manage their pain and get them off opioids, it’s going to be fabulous,” Doorenbos said.
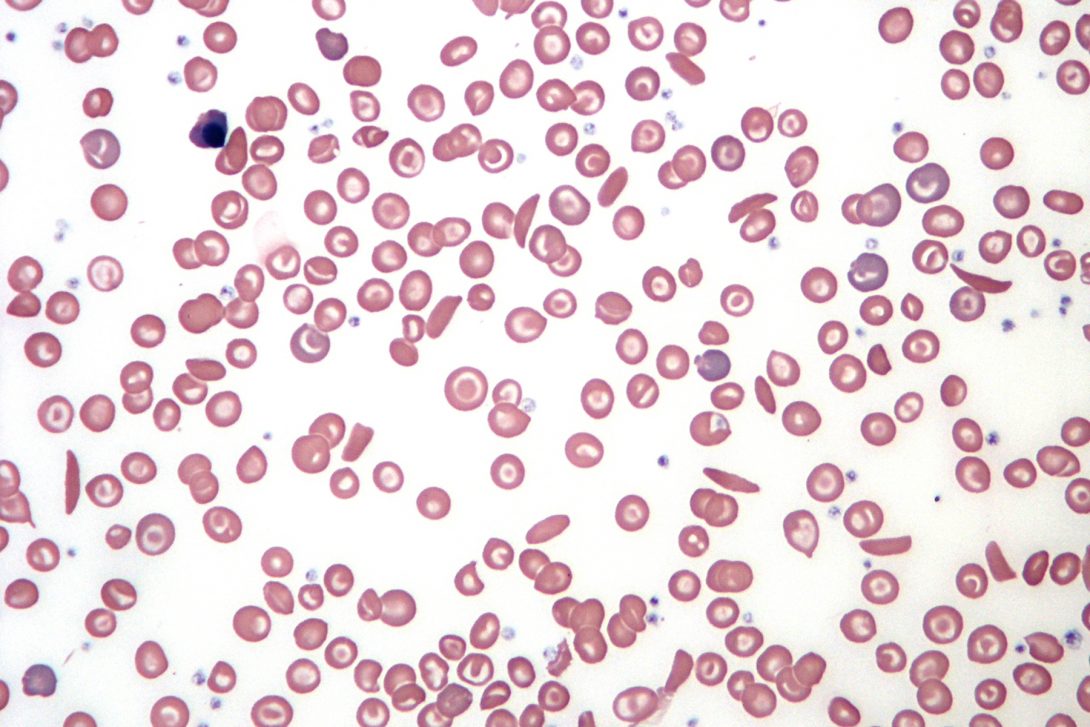
Sickle cell disease affects as many as 100,000 people in the U.S. and at least 20 million worldwide, according to researchers. The disease is an inherited defect of the hemoglobin that causes the red blood cells to become crescent-shaped. These cells can lyse and obstruct small blood vessels, depriving the body’s tissues of oxygen. The disease can cause extreme pain and damage the lungs, heart, kidneys and liver. Stroke and other complications can be life-threatening. In the U.S., the genetic disorder strikes mainly African Americans.
Dr. Robert Molokie, UIC clinical associate professor of medicine and co-principal investigator on the project, explained there are many things that can cause issues and trigger a pain crisis for those with SCD, including stress and even changes in the weather.
body
Pain is SCD’s hallmark symptom and the leading cause of almost 200,000 annual emergency department admissions. It is also the leading cause of hospitalization for those with SCD, with an estimated $2.4 billion in annual U.S. healthcare costs, according to the American Journal Hematology. Pain, both acute and chronic that is so severe that it requires opioids to attempt to keep it to tolerable levels, is a constant companion to those living with SCD.
Doorenbos and her team will conduct a hybrid type 1 effectiveness implementation trial to assess the effectiveness of acupuncture and guided relaxation on people with SCD while observing and gathering information on implementation in three health systems: University of Illinois Hospital & Health Sciences System, University of Florida Health and Duke University Health Systems. Each serves a large population with SCD and uses EPIC as their electronic health record, which will facilitate data gathering and analysis.
For the study, 360 SCD patients will receive acupuncture twice a week for five weeks. Judy Schlaeger, associate professor in the Department of Human Development Nursing Science, who developed an SCD treatment plan, determined that the time frame allows for a successful impact on pain. Also, patients will be asked to use guided relaxation techniques at least once a day. These techniques, which patients access via smartphone or computer, were developed by Miriam Ezenwa, a University of Florida associate professor in biobehavioral nursing science. Both acupuncture and guided meditation were proven effective in pilot studies on SCD pain management.
One aim of the study is to discover which non-pharmacological pain management interventions work best for SCD patients and how to make these treatments regular practice at the three research health systems involved in the study.
Because SCD is genetic, many patients are diagnosed in childhood or young adulthood. Managing their pain is critical to their development.
“What makes the pain so problematic is it causes a lot of missed school days. If we don’t manage the pain, that can affect their education,” said Doorenbos, who added that the pain often continues to impact their working life as adults.
“If we can better manage the pain, we could impact the quality of life and change the possibilities for SCD patients. They can have a plan for activities and have a more productive work situation. Pain management can change so many things in their life,” Doorenbos said.
The researchers will be working with patients with sickle cell disease in the fall of 2021, pending additional approvals from the UIC Institutional Review Board.
Doorenbos, Molokie and Schlaeger are principal investigators for NIH grant UG3AT011265. They are joined by Dr. Nirmish Shah (Duke University) and Miriam Ezenwa (University of Florida).