Improving access to services for sexual assault survivors
Julie Brosnan, DNP '23, RN
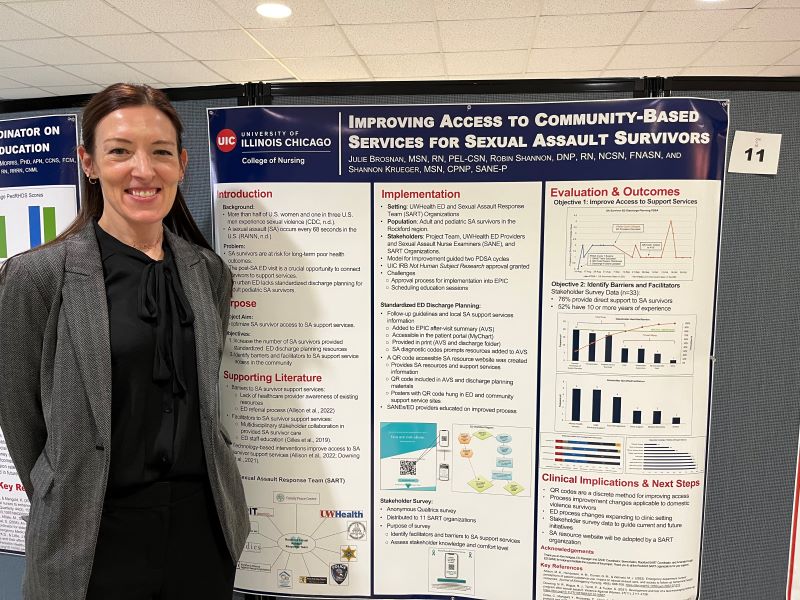
Clinical Issue/Practice Problem: In the U.S., a sexual assault (SA) occurs every 68 seconds. Without proper follow-up care, SA survivors are at risk for long-term poor health outcomes. Emergency department (ED) encounters are often the only healthcare encounter for SA survivors. An urban university health system lacks standardized ED discharge planning for survivors. This quality improvement project aims to 1) increase survivor access to SA support services and 2) identify barriers and facilitators to accessing support services.
Summary of Supporting Literature: Previous studies indicate staff education and technology-based interventions are effective in optimizing care and survivor accessibility to resources. Evidence supports an assessment of stakeholder knowledge and input to inform community SA response efforts.
Project Implementation: The Model for Improvement guided two Plan-Do-Study-Act Cycles. Implementation included (a) creation of a QR code accessible SA resource website, (b) ED standardized SA survivor print and electronic (EPIC) after-visit summaries with follow-up guidelines and the QR code, (c) ED staff education, and (d) a community stakeholder survey to assess facilitators and barriers to support services.
Outcomes: During PDSA Cycle 1, 19 survivors were seen in the ED and 14 SA resource website visits. During PDSA Cycle 2, 13 SA survivors were seen in the ED and 29 website visits. Stakeholder survey data revealed barriers to support services were transportation, overloaded support services, and survivor knowledge of existing services.
Clinical Implications/Next Steps: The ED has adopted standardized SA survivor discharge planning and is expanding to the clinic setting. The local multi-agency sexual assault response team will employ stakeholder survey data to improve SA survivor access to community resources.