Improving mobility rates
Helen Miranda, DNP '23, RN Heading link
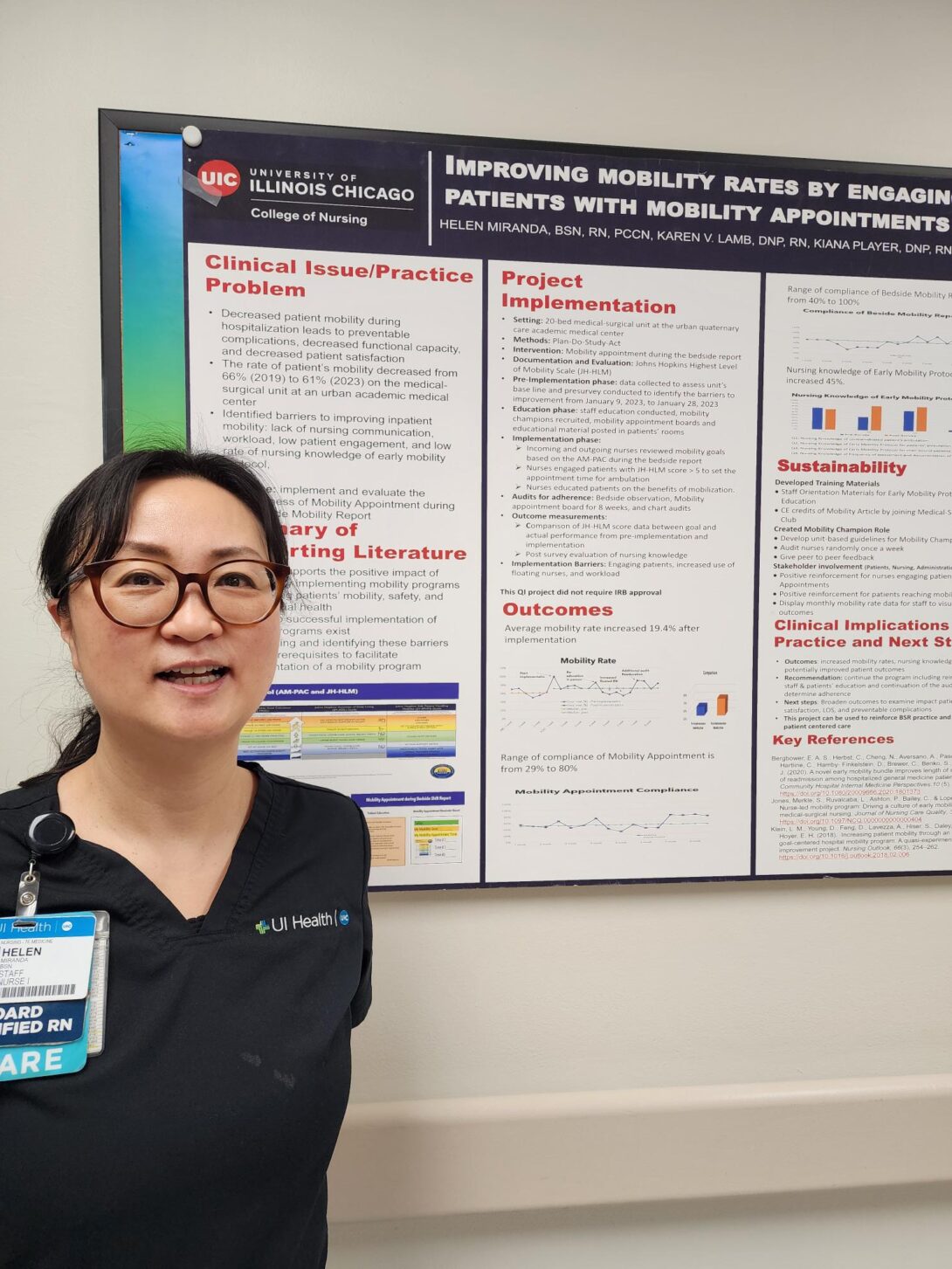
Clinical Issue: Decreased patient mobility during hospitalization leads to preventable complications, decreased function, and decreased patient satisfaction. The rate of patient’s mobility decreased from 66% (2019) to 62% (2023) on the medical-surgical unit at an urban academic medical center. Identified barriers to improving inpatient mobility are lack of patient motivation, low rate of knowledge of early mobility protocol, and lack of nursing communication. The purpose of this project was to implement and evaluate the effectiveness of Mobility Appointment during the Bedside Mobility Report (BSR).
Supporting Literature: Evidence supports the positive impact of successfully implemented mobility programs in improving patients’ mobility, safety, and psychosocial health. However, barriers to successful implementation of mobility programs exist. Understanding and identifying these barriers are key prerequisites to facilitating implementation of a mobility program.
Project Implementation: Roger’s Diffusion of Innovation Theory provided the framework to adopt the mobility appointment project. A pre-survey was used to identify the barriers and nursing knowledge in early mobility protocol. The mobility goal was reviewed in staff education. Bedside mobility reports observation audit tools, and mobility appointment board audits were utilized to collect staff compliance. Engaging patients and nurses’ project adoption was challenging.
Outcomes: The mobility rate was improved 19.4% with 45% improvement of the nursing knowledge of early mobility protocol after implementation.
Clinical Implications: This QI project identified the keys to adoption among nurses to improve the mobility rate. This project can be used to reinforce BSR practice and promote patient centered care.